Many relevant diagnostic signs are not performed deliberately by the examiner or by the patient at the examiner’s direction. They are observed as the patient reacts to their condition. Fortin’s finger sign, Minor’s sign, and Vanzetti’s sign are three examples of this principle.
Infrared Thermal Imaging of Temporomandibular Joint Syndrome
Temporomandibular joint (TMJ) syndrome is a common problem encountered in clinical practice. Signs and symptoms of TMJ syndrome can include pain on opening the mouth, trismus, joint clicking and noises, pain on chewing, headache, TMJ tenderness to palpation, auriculotemporal paresthesias, pain in the neck, pain/fullness sensation in the ear, and tinnitus. Pain may be unilateral or bilateral with palpable tenderness. Patients may present with a combination of structural dysfunction due to ligament/capsular/discal derangement and/or myofascial involvement due to trigger points of the masseter, temporalis, and pterygoids.
TMJ syndrome may occur as a result of the cervical acceleration/deceleration syndrome, as well as other structural problems such as posture, stress, with or without bruxism, malocclusion, leg length discrepancy, and blunt trauma. A full discussion of the TMJ syndrome is beyond the scope of this paper, but when a patient presents with the above signs and symptoms, the treating doctor should have a high index of suspicion for TMJ syndrome.
Diagnostic imaging of the TMJ includes radiographs of the TMJ, open and close-mouthed, as well as panorex views. MRI may be helpful to diagnose structural abnormalities such as torn temporomandibular ligaments or anteriorly displaced disc. A cost effective, non-invasive, risk free, imaging tool that may be utilized is thermography. While x-ray and MRI can show structural/morphological aspects of the TMJ syndrome, thermography can show physiological information with reference to dysautonomia associated with TMJ as well as myofascial pain dysfunction (MPD) and trigger points. Thermography is recommended as one of the diagnostic tools useful for TMJ syndrome by the American Academy of Head, Neck, and Facial Pain and TMJ Orthopedics published in a position paper in Cranio: The Journal of Craniomandibular Practice in January 1990.
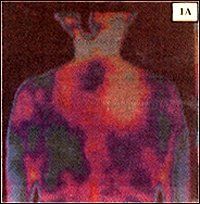
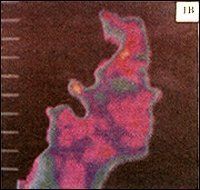
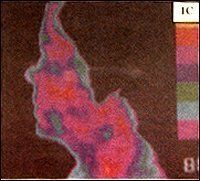
In a paper published in the Clinical Journal of Pain in 1987, by Weinstein, et al., a TMJ protocol was described for thermographic imaging of the facial area in patients with TMJ syndrome. In their study of 200 patients with TMJ symptoms they found a 95 percent correlation between the anatomical distribution of symptoms and thermographic findings. Their TMJ protocol included using a one-half degree level of sensitivity and a one-half degree delta T (temperature differential) from right to left. They recommended a triplicate series of facial views including; frontal, right and left lateral facials, trigger point views of the anterior cervical spine, posterior cervical spine, and interscapular region. Weinstein's criteria finds a positive study when:
- The affected joint is a 1.0 degree centigrade warmer then the opposite side in comparison to the ambient room temperature.
- Each affected masseter is 1.0 degree centigrade below ambient room temperature.
- Location of the pain pattern matches the pain diagram.
In a study published by Pamela Steet, D.D.S., and published in the Journal of Craniomandibular Practice, she found thermography to be very useful in the diagnosis and management of TMJ syndrome. She found a 94.5 percent sensitivity using thermography for TMJ syndrome, which correlates well with the Weinstein study. After treatment, thermography was able to assess the successful outcome of treatment in 80 percent of the cases. She was also able to find a pattern that could differentiate acute vs. chronic TMJ dysfunction.
In another study, published by Weinstein, they documented normal temperature differences in the face (Table 1). They also found that 0.5 degrees Celsius difference from right to left of the face had a 96 percent confidence level for underlying pathology.
Table I | |||
Mean Skin Surface Temperature Value Differences: Male vs. Female | |||
Mean Difference | Mean | Mean | |
| Muscle | Male vs. Female(oC) | Male(oC) | Female(oC) |
| L. temporalis | 0.7 | 37.18 | 37.12 |
| R. temporalis | 0.5 | 37.24 | 37.18 |
| L. frontalis | 0.1 | 37.07 | 37.18 |
| R. frontalis | -- | 37.11 | 37.15 |
| L. peripunctal area | 0.2 | 38.4 | 38.19 |
| R. peripunctal area | 0.22 | 38.38 | 38.15 |
| L. front masseter | 0.27 | 35.96 | 35.69 |
| R. front masseter | 0.36 | 36 | 35.64 |
| L. mentum | 0.06 | 36.93 | 36.99 |
| R. mentum | 0.07 | 36.94 | 37 |
| L. sup. temporal artery | 0.02 | 37.99 | 37.77 |
| R. sup. temporal artery | 0.21 | 38 | 37.79 |
| L. temporomandibular joint | 0.4 | 37.12 | 36.72 |
| R. temporomandibular joint | 0.6 | 37.09 | 36.7 |
| L. lateral masseter | 0.39 | 36.4 | 36.02 |
| R. lateral masseter | 0.41 | 36.44 | 36.02 |
Summary of TMJ findings with infrared imaging:
- Focal hyperthermia over the TMJ
- Focal, hot spots consistent with trigger points at the paracervical, interscapular, suprascapular regions, and the masseter region
- Decreased thermal emission over the masseter muscle area
- Increased thermal emission over the temporalis muscle area
Conclusion
Thermography is a useful diagnostic imaging tool available to the treating doctor to differentially diagnose this multifaceted complex syndrome from other conditions with similar symptoms. The TMJ syndrome has a distinct thermal pattern. Thermography is also useful to help follow the patients' response to treatment.
David BenEliyahu, D.C., DNBCT
Selden, New York



