Spearheaded by burgeoning scientific and clinical research literature, psychedelics have reached a level of media coverage and popular interest that has not been seen for over half a century. By “psychedelics,” we are referring to the unique class of substances that includes psilocybin (the active compound found in so-called “magic mushrooms”), LSD, dimethyltryptamine (DMT), ayahuasca, 5-MeO-DMT, and mescaline – each of which occurs in the natural world (except for LSD, which is a semi-synthetic compound).
Abdominal Calcifications Review
The key to identifying calcifications in the abdomen is knowing the anatomy. I'd like to review some of the more common findings and give a method of viewing each quadrant.
First, consider the pattern, and then consider what anatomical structure is in that location. Four basic appearances are seen with calcifications in the abdomen, generally described as:
- rim-like;
- linear or track-like;
- lamellar; and
- cloud-like.
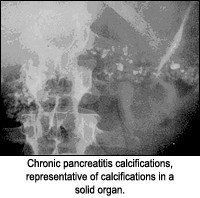
Rim-like appearance can be described as a wall of calcification surrounding a hollow structure, as in a renal cyst. Track-like or linear calcification indicates a tubular structure, as in the walls of the ureters or arterial walls. Lamellar calcification is formed in the lumen of a hollow structure, as in renal stones or stones in the gallbladder. Cloud-like calcifications are formed in a solid organ or tumor, such as a leiomyomas of the uterus or calcifications in the pancreas. Once the appearance of the calcification is apparent, the next step is to consider what anatomical structure is in that location. I am assuming one has ruled out the possibility of an artifact before considering a calcification as such.
The structures most commonly associated with calcifications are the following (based on their respective quadrant):
- Right upper quadrant: liver, biliary tract including gallbladder, kidney and adrenal gland.
- Left upper quadrant: spleen, kidney, adrenal and splenic artery.
- Left lower quadrant: phleboliths, mesenteric lymph nodes, ovary, renal ureters, iliac artery.
- Right lower quadrant: appendix, phleboliths, mesenteric lymph nodes, ovary, ureters, iliac artery.
- Lower abdomen median: aorta, uterus, bladder and prostate.
- Upper abdomen median and paramedian: pancreas.
The following images are representative of the four classic appearances of calcifications (rim-like, linear, lamellar, and cloud-like):




Normal Calcifications
Bones are the only normal calcified structures. However, many other calcifications will be seen that have no clinical significance:
- vascular veins of the pelvis (phleboliths). Calcified thrombi within the deep veins of the pelvis should be dismissed as soft-tissue variants simulating stones of the genitourinary tract. Most of these clinically insignificant anomalies will be found lateral to the bladder walls and appear as nodular, homogenous opacities.
- costal cartilage
- lymph nodes (calcified mesenteric lymph nodes are common)
- granulomas
- injection sites
Renal calculi sometimes can be confused with mesenteric lymph node calcification or phleboliths, depending on location. The kidney calculi are frequently found in the lower end of the ureter, where it turns to enter the bladder. Other locations are the uretero-pelvic junction and where the ureter crosses the iliac vessels in the pelvis. An estimated 80 percent of all kidney and ureteral stones are visible on plain films. Unfortunately, this is technique-dependent.
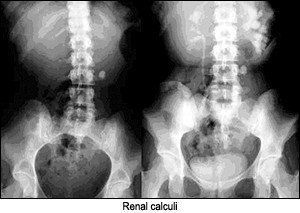

Other shadows and opacities that need to be differentiated are material in the bowel, such as fecal masses, undigested supplements, enterolithes, bismuth, and barium, particularly in the diverticula of the colon, which can mimic kidney calculi or other calcifications. The appendix often lies in close relationship to the right ureter, and enteroliths within the appendix may be mistaken for ureteral calculi. Even the tip of the transverse process of a vertebra may appear as a greater density than the vertebral body, suggesting a possible calculus.
Calcifications in uterine fibroids appear as a collection of berries and generally are not difficult to differentiate from other calcifications in the pelvis.

I have not listed all of the possible calcifications that can be seen in the abdomen, just the more commonly seen calcifications. Most calcifications can be identified using the four-quadrant method and using the appearance of the calcification to determine the location. Of course, good film quality is a must.
Deborah Pate, DC, DACBR
San Diego, California
patedacbr@cox.net



