Spearheaded by burgeoning scientific and clinical research literature, psychedelics have reached a level of media coverage and popular interest that has not been seen for over half a century. By “psychedelics,” we are referring to the unique class of substances that includes psilocybin (the active compound found in so-called “magic mushrooms”), LSD, dimethyltryptamine (DMT), ayahuasca, 5-MeO-DMT, and mescaline – each of which occurs in the natural world (except for LSD, which is a semi-synthetic compound).
Aggressive Conservative Treatment Not Helpful for Frozen Shoulder
One of the most difficult conditions to treat is adhesive capsulitis or "frozen shoulder." In many cases, this condition is self-limited in one to two years, but sometimes, a residual stiffness continues for years. The condition is said to go through three phases. First, the "freezing" or acute painful phase, during which the pain may begin at night and continue during the day, unrelated to motion. There may be more pain at rest. During this phase, the patient may be comfortable with the arm at the side with internal rotation. This position relaxes the tension of the inflamed glenohumeral capsule, biceps and rotator cuff. Unfortunately, just resting this type of shoulder and limiting motion leads to increased stiffening.1 Rowe stated that treatment consisting of exercise or manipulation in this phase prolonged the condition and sometimes created permanent damage.2
In the second stage, progressive stiffness occurs, resulting in the "frozen shoulder" diagnosis. During the first stage, which is inflammatory, it is very difficult to predict that the patient will end up with a frozen shoulder. According to Cyriax's capsular pattern, the most limited motion in the frozen stage is passive or active lateral rotation, followed by limited glenohumeral abduction and finally, limited internal rotation. The final stage of "thawing" results in a slow gain in motion or comfort. The first stage may last between two and 9 months; the second phase between three and 12 months; and the final stage four weeks to three or more months.
Recently, a study was performed3 to prove the hypothesis that treating patients with supervised neglect can attain painless and better range of motion within a shorter time span than by means of intensive physical therapy with passive stretching and mobilization, which created pain. Patients with diabetes mellitus were excluded, since they have a different course of the syndrome than normal patients and are more resistant to all types of treatment. Diabetics often show bilateral shoulder involvement, and the longer they have been on insulin the higher the risk of developing shoulder stiffness.
The study involved two groups of adhesive capsulitis patients. Patients in both groups lost more than 50 percent of motion of the glenohumeral joint in all directions for three months or more. One group was told not to exercise in excess of their pain threshold; to perform pendulum exercises and active exercises within this painless range; and to only perform activities that were painless. The second group was given active exercises up to and beyond the pain threshold, passive stretching and manipulation of the glenohumeral joint, and home exercises with maximal stretching and reaching. Neither group received corticosteroids, manipulation, or mobilization under anesthesia. The study concluded that supervised neglect yielded better outcomes than intensive physical therapy and passive stretching in patients with frozen shoulder. The authors questioned the high percentage of results published in which manipulation under anesthesia and arthroscopic or open release were used, since these interventions are usually performed after a year of intensive physical therapy, and the surgical patient feels better after three months, which is often the normal self-limiting period of involvement.
Treatment of adhesive capsulitis depends on the stage of the disease. In the acute stage, most treatments, including manipulation, injections, anti-inflammatory medications, heat, rest, ultrasound, and acupuncture, do not help. Rowe found that in the acute phase, adhesive capsulitis patients responded best without any form of treatment, except for pain medication as needed and use of the arm as much as possible without pain.
Joint-play manipulation of the shoulder usually exacerbates the condition, especially in the first two stages of the condition. Active Release®, Graston Technique® or prolonged fascial release without creating pain helps to release the anterior capsule in the second and third stages. These techniques must not be used if they are creating more than an ache. The use of prolonged, low-intensity stretching at elevated tissue temperature, followed by cooling of the tissue, is beneficial. This technique allows the plastic deformation necessary to free the adhesed capsule.
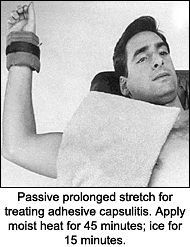
This procedure (see figure above) works well at home for the patient who lies supine with the shoulder in external rotation and 90 degree abduction, covering the anterior capsule with moist heat, while holding a 1 to 2 pound weight and maintaining the stretched position for up to 45 minutes. If there is pain, the weight should be reduced, or in the beginning, just the weight of the arm may be adequate. The patient can feel discomfort, but not pain. Ice is applied during the last 10 to 15 minutes, maintaining the lateral rotated arm position. The ice apparently fixes in the new increased range of lateral rotation. Thus, it is clear that painful stretching or joint play is not indicated for the treatment of adhesive capsulitis.
References:
- Harryman DT, Lazarus MD, Rozencwaig R. The Stiff Shoulder. In: Rockwood CA, Matsen FA. The Shoulder. Philadelphia, WB Saunders Co., 1989:1064-1112.
- Rowe CR. The Shoulder. New York, Churchill Livingstone, 1988:155-163.
- Dierchs RL, Stevens M. Gentle thawing of the frozen shoulder: a prospective study of supervised neglect versus intensive physical therapy in seventy-seven patients with frozen shoulder syndrome followed up for two year. J Shoulder Elbow Surg 2004;13(5):499-502.
Warren Hammer, MS, DC, DABCO
Norwalk, Connecticut
softissu@optonline.net
www.warrenhammer.com



