Spearheaded by burgeoning scientific and clinical research literature, psychedelics have reached a level of media coverage and popular interest that has not been seen for over half a century. By “psychedelics,” we are referring to the unique class of substances that includes psilocybin (the active compound found in so-called “magic mushrooms”), LSD, dimethyltryptamine (DMT), ayahuasca, 5-MeO-DMT, and mescaline – each of which occurs in the natural world (except for LSD, which is a semi-synthetic compound).
The Hip Joint - Another Perspective: Intraosseous Restrictions of the Neck of the Femur
There are significant differences between the extremities and the spine. For one, the bones of the extremities are primarily long bones. Long bones, especially those that bear weight, have a tendency to become stiff and develop intraosseous restrictions, whereby the bone itself lacks flexibility and give. Bones are not the dead, calcified structures we worked with in a cadaver lab; they are live tissues, full of blood and a protein matrix, designed to have a certain degree of flexibility and movement. (I explored this concept in an earlier article, available online at: www.chiroweb.com/archives/19/23/12.html.) These restrictions respond well to low-force adjusting.
Adjusting bones, rather than joints? Has Marc gone off the deep end? No. The concept: All connective tissue structures are built similarly. They all have the same cellular structure. The intracellular structure is based on the structural integrins, making the cell more than a bag. The cellular memories of trauma or of a persistent postural positioning or misuse can be stored in bony tissue. George Roth's Web site (www.rothinstitute.com) has a series of articles that explain the science behind this concept. All connective tissues are more similar than different from one another. All connective tissues can respond similarly to distress. The response is expressed as tightness and restriction. "My gut knotted up" is a reality, not just a metaphor. What tissues does this broader concept of subluxation apply to? I would include the bones, the ligaments and fascia of the musculoskeletal system and the viscera, the muscular lining of the blood vessels, and the perineural lining of the nerves.
All of these tissues can develop restrictions that need to be addressed to resolve chronic problems. The scientist in me reminds you that these ideas are speculative and theoretical, and that there are only limited studies supporting these techniques. The peer- eviewed-level research that speaks of related phenomena shows that on bone bruises, injuries to bones that are less than a complete fracture are detectable on MRI. I have listed one such article in my sources. The clinician in me has been using these ideas for eight years with great success, and knows that they are grounded in reality and clinically effective.
Let's get practical and apply this concept to one particular structure: the neck of the femur. This technique is taken directly from George Roth's work. The inferior part of the femur is vertical, and then turns in a medial direction at the trochanter, heading toward the acetabulum of the pelvis. This short bone and its restrictions are quite significant for pelvic and hip problems.

When restricted, the bony prominence of the greater trochanter will be tender to the touch. The medical diagnosis might be "trochanteric bursitis." I would disagree with this term, and say that the bursal inflammation is usually secondary.
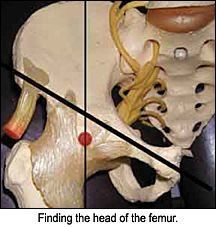
To screen for this intraosseous restriction, push at an oblique upward angle directly along the axis of the neck of the femur, from the greater trochanter directly toward the acetabulum. You can determine this angle by marking the spot where the femur head meets the acetabulum. Find this spot by first locating the midpoint of a line from the ASIS to the pubic symphysis. Drop inferior from this point by one centimeter, and feel for the palpable bony head of the femur. Another assessment tool can be used to locate the axis of the neck of the femur. Press obliquely upward at the greater trochanter, feeling for the exact direction that gives you the sense you are pressing directly through bone. Even in a normal, nonrestricted femoral neck, you will have a feeling of substance; of a push through bone. If you change your direction by 5 degrees, the feeling is much more empty. This compressive motion is your basic screen. Is there normal give here, or is the bone restricted? You can use a leg check or muscle test to confirm, if that is your style. If you are using strictly palpation, you will need to develop an experience database, feeling many of these before you fully own the technique.
Once you have established that this compression test is abnormal, test for the three basic directions of restriction involving the neck of the femur. One would be an abnormal degree of linear expansion along the axis of the bone, based on the compression test outlined above. This means that the bone is functionally lengthened along its long axis. The second lesion would be a compression, which means the bone is functionally shortened along its long axis. Test by pulling the bone obliquely outward and inferior, along the same axis. Test for this with contacts on both the anterior and posterior surface of the greater trochanter. I use my whole hand for this contact, and pull with my whole body, not just from my wrists. The third possible lesion is a radial expansion of the greater trochanter. This is an expansion of a "knobby" area; in this case, the greater trochanter. Imagine or look at the expanded tibial plateau of a severely degenerated knee to get a sense of what kind of bony remodeling can occur in this type of structure.
You would test this by surrounding the greater trochanter with two hands, and pushing your hands together at heller.various angles, looking for the direction of maximal resistance.
The correction follows from the assessment. For a compressed femur, use Engage, Listen, Follow (ELF) to gradually pull the neck of the femur obliquely outward and inferior. For expansion, use either ELF or recoil (engage/release). For a radial expansion, either of these techniques can be used. This is a dense, two-inch-long part of the bone, so the correction may require significant pressure. I use a percussor, pressing it medially over the gluteus medius, just above the greater trochanter, to help me with all of these techniques. If you have this instrument, or something similar, it makes the job easier, by softening all of the tissues in the area. For a compressed neck of femur, where I want to use both of my hands to pull the bone outward and inferior, I will have the patient hold the percussor. Due to the density of the bony tissue, it takes a while for the release to begin. Engage, and after a few seconds of delay, the tissue will begin to release.
Once you master this assessment and technique, you will be amazed that you actually practiced without it for years. This model of assessment of intraosseous lesions is something I use on every patient, and I will further explore it as I cover more areas of the extremities in this series.
The neck of the femur is a very clinically significant area. I do this adjustment almost every day. I find this lesion coexisting with sacroiliac problems, with any lower extremity problem, and with pirformis tightness. I invite you to continue to expand your "toolbox," and remain excited about your work. Your patients will share this excitement, and will respond and refer.
Resources
- Matrix Repatterning seminars (George Roth), 2001.
- Mechanical Link seminars (Paul Chauffour), 1997-2001.
- Chauffour P, Prat E. Mechanical Link: Fundamental Principles, Theory, and Practice Following an Osteopathic Approach. North Atlantic Books, 2002.
- Graf BK, Cook DA, De Smet AA, Keene JS. "Bone bruises" on magnetic resonance imaging: evaluation of anterior cruciate ligament injuries, American Journal of Sports Medicine March-April 1993: [url=http://www.findarticles.com/p/articles/mi_m0918/is_n2_v21/ai_13715443]http://www.findarticles.com/p/articles/mi_m0918/is_n2_v21/ai_13715443[/url].



