Many relevant diagnostic signs are not performed deliberately by the examiner or by the patient at the examiner’s direction. They are observed as the patient reacts to their condition. Fortin’s finger sign, Minor’s sign, and Vanzetti’s sign are three examples of this principle.
Complex Regional Pain Syndrome
Complex regional pain syndrome (CRPS) is the new title that has been advocated for reflex sympathetic dystrophy syndrome and causalgia by the International Association for the Study of Pain. A new taxonomy has been suggested because not all cases have "sympathetic maintained pain" (SMP), and not all cases demonstrated dystrophy. These conditions usually follow a precipitating injury that does not heal as expected, and is often accompanied by unrelenting pain that is out of proportion to the initial injury.
There have been two categories of CRPS described: Type I, and Type II. Sympathetic maintained pain (SMP) may or may not be found in association with CRPS, and is characterized by pain that is maintained by sympathetic innervation or circulating catecholamines. SMP can be abolished by sympatholytic agents.
Complex Regional Pain Syndrome, Type I
CRPS Type I is a syndrome that develops after a precipitating noxious injury or event. It is not limited to any particular nerve and tends to extend regionally beyond the focal area of injury. It may be associated with any or all of the following: edema, vasomotor disturbances, allodynia, hyperesthesia, and sudomotor dysfunction. It may follow a fracture, soft tissue injury, or even immobilization from angina or stroke. The symptoms typically start about one month after the precipitating injury or event, and is often described as burning and unrelenting pain exacerbated by movement and light touch. Abnormalities in blood flow can occur and may include changes in skin temperature and color, making infrared thermal imaging and triple phase bone scans useful lab tests in identifying CRPS. Atrophy of the skin, nails, and hair may be seen with hyper or hypohydrosis. Edema is usually present with loss of joint mobility. Impaired motor function with tremors and weakness can be observed as well.
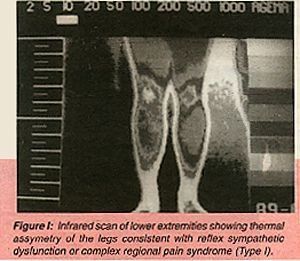
Lab findings can include temperature assymetry (hot or cold) of greater than 2.0 degrees centigrade, as seen on infrared thermal imaging (Fig. I). However due to unstable vasomotor changes often seen, imaging at different times can be necessary. Triple phase bone scans (TPBS) are very sensitive, and specific for CRPS-Type I and show different findings in each of the three phases, with a characteristic periarticular uptake in the "blood pool" or static phase of the TPBS (Fig. II). This type of CRPS was previously called RSDS.

Complex Regional Pain Syndrome, Type II
Type II is defined by burning pain, allodynia, and hyperpathia usually in the hand or foot after peripheral nerve injury. Onset usually occurs after nerve injury but may be delayed. The most common nerves involved include the median, ulnar, sciatic, and tibial. Pain is constant and burning and is exacerbated by light touch, stress, temperature, movement of the limb, and emotional disturbances. Abnormalities in skin temperature, and blood flow may occur as well as sudomotor dysfunction. Dystrophic changes may occur in the skin, hair or nails. This type of CRPS was previously referred to as "causalgia."
A therapeutic ladder was suggested by Racz et al., from the Texas Tech Center Dept. of Anasthesiology.
(I) TENS, opioids, medication, biofeedback, psychotherapy, physiotherapy, patient education, manipulation, etc.
(II) Sympathetic blocks, or IV drip blocks
(III) Sympathectomy or neurolysis
The earlier CRPS is recognized, the better the chances are of therapeutic success. Therapy should be multidisciplinary, and the doctor of chiropractic should refer these patients for concurrent medical and psychotherapy.
Reference
Tollison and Satterthwaite. Sympathetic pain syndromes -- RSD and causalgia. State of the Art Reviews: Physical Medicine and Rehabilitation, 10(2), June 1996.
David BenEliyahu, DC, DACBSP
Selden, New York



