Many relevant diagnostic signs are not performed deliberately by the examiner or by the patient at the examiner’s direction. They are observed as the patient reacts to their condition. Fortin’s finger sign, Minor’s sign, and Vanzetti’s sign are three examples of this principle.
A Description of the Common Compensatory Pattern in Relationship to the Osteopathic Postural Examination
Postural evaluation is an integral part of a comprehensive musculoskeletal work-up. Many methods have been developed to assist the physician with this most fundamental task. A number of decades ago, a device which used plumb and level lines was developed to assess anatomical asymmetry in the standing patient. More recently, the use of bilateral scales has been employed by certain practitioners to determine load-bearing imbalances side-to-side and front-to-back. Very recently, sophisticated computer software programs have been developed and applied to the previously mentioned diagnostic designs to make it possible for the examiner to objectify multiple parameters related to the postural examination.
The upright postural evaluation methodology common to the clinical disciplines of osteopathy, chiropractic, and allopathy is inherently limited:
- It requires the patient to assume an erect weightbearing position. For many patients this position would be difficult or even impossible.
- For the minimal amount of information obtained, it is time consuming.
- Modern analytic equipment can be expensive.
- It does not conclude with sufficient information necessary to allow the practitioner too correct existing articular lesions.
Early on the osteopathic profession saw the need for an inexpensive, reproducible and expedient method to assess postural imbalances and related somatic dysfunction. The system which has been developed provides decided advantages. It does not require the patient to be upright or weightbearing, is quick, and requires no extraneous equipment. Once the evaluation has concluded, the clinician has adequate information about postural imbalance and somatic dysfunction, and can apply manual manipulative techniques in a corrective manner.
Certain osteopathic physicians have observed clinically that a significant percentage of the population assumes a consistently predictable postural adaptation, arising from nonspecific mechanical forces such as gravity, gross, and micro-trauma, and other physiological stressors in the external milieu. These forces have their greatest impact on the articular facets in the transitional areas of the vertebral column. Citations in the osteopathic literature refer to this postural adaptation as "the common compensatory patter" (CCP). The CCP has been the subject of the writings of Zink, 1979; Johnson, 1988; Ellestad et al., 1989; Johnson and Cross, 1990; and Cross and Johnson, 1990.
In the CCP, an examiner will note the following observations will apply to the supine patient. The left leg will appear longer than the right. The left iliac crest will appear higher or more cephalad than the right. The pelvis will roll passively easier to the right than to the left because the lumbar spine is sidebent left and rotated right. The sternum is displaced to the left as it courses inferiorly. The left infraclavicular parasternal area is more prominent anteriorly because the thoracic inlet is sidebent right and rotated right. The upper neck rotates easier to the left. The right arm appears longer than the left, when fully extended. While the CCP will be observed most often during examination, we will also note that variations do occur from patient to patient. These variations from the CCP were referred to by Zink as disparent patterns.
While postural examination techniques in the supine position appear to be fully appreciated within the osteopathic profession, the concept of the CCP may still be largely under-recognized. This paper represents a further attempt to describe the CCP in relationship with the osteopathic postural examination.
Observation of the Common Compensatory Pattern during the Osteopathic Postural Evaluation
The focus of this paper is to demonstrate the CCP, while utilizing the osteopathic postural examination as a diagnostic procedure upon which diversified manipulative techniques could be readily applied. Therapeutic manual techniques will not be demonstrated in this article. Various and sundry manipulations will be readily inferred by experienced clinicians as they read the general listings.
The examination procedure is undertaken with the patient supine. The patient should be comfortable and modestly draped. The physician should make proper use of the dominant hand and eye so as to arrive at an accurate diagnosis. The examiner begins by comparing the length of the legs bilaterally, standing at the foot of the table facing the patient. In the CCP, the left leg will appear to be longer, as compared to the right.
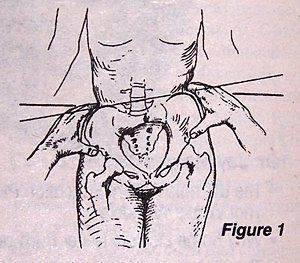
Next, the examiner compares the height of the innominates by moving to the side of the table and placing the lateral aspects of the hands immediately over the prominence of the crests. Slight medial pressure may be required in the obese patient to adequately visualize these landmarks. In the CCP, the left crest is more cephalad than the right, due to the left sidebending of the lumbar spine (Fig. 1).
At the same time, the doctor should hook the thumbs just under the anterior superior iliac spies (ASIS) to assess variation bilaterally (Fig. 1). If the patient is in the CCP, the ASIS on the left should appear relatively superior. This information suggests that the left innominate is rotated posteriorly and inferiorly if we were using the posterior superior iliac spine (PSIS) as a reference.
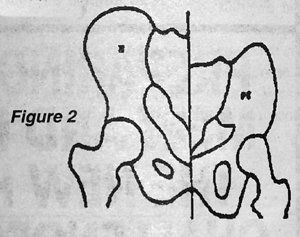
Figure 2 schematically demonstrates how the left innominate would appear radiographically as compared to a neutral posture. At this point, the physician should attempt to rotate the pelvis of the patient, rocking first to the right and then to the left (Fig. 3 & 4). The side to which the pelvis rocks with the least resistance suggests the general rotation of the motion segments between the lower lumbars and the sacrum.
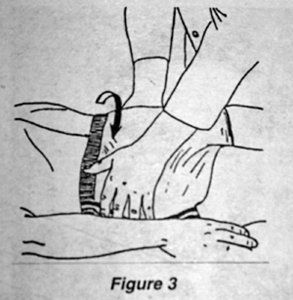

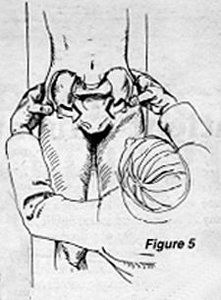
The physician should also palpate the lumbar paravertebral musculature for tautness and tenderness. In the CCP, the pelvis will more readily rotate to the right and the left paraspinal soft tissues will appear more contracted and perhaps more tender to palpation (Fig. 5).
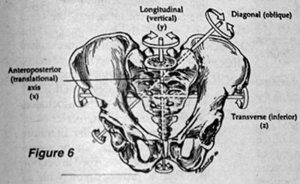
These findings and the relative elevation of the left crest noted earlier indicates that the lumbars are in a right rotary malposition and the sacrum is malpositioned such that there is a left rotation on the left oblique axis (Fig. 6).
The sacral base is tilted to the right (Fig. 7). Secondarily, we may also conclude that the lumbar spine is sidebending to the left, forming a mild dextroscoliotic curve apexing at approximately L3.

Upon visualization and palpation, the lower thoracic cage will appear to rotate or deviate to the left and the thoracic spine will gradually sidebend to the right, forming a mild levoscoliotic curve, in CCP, as it compensates for the lumbar and pelvic somatic adaptations. These changes suggest that the thoracolumbar transitional area is rotated left (Fig. 7) and sidebent right.
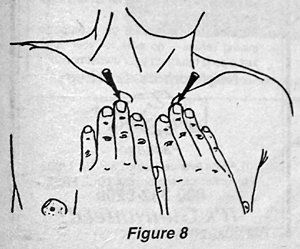
Now the physician should palpate the infraclavicular parasternal area with the pads of the fingertips (Fig. 8). In CCP, the left infraclavicular parasternal area is more prominent or convex and resists manual pressure to a greater degree than its contralateral side. It may also be more tender to touch.
The articulation of the first rib with the sternum is a synchondrosis and, as such, it reflects rotation in the first thoracic vertebra (T1). In CCP, T1 is rotated right and this forces the left infraclavicular parasternal region to be more prominent on the left side.
At this point, the examiner moves to the head of the table and applies gentle pressure in an inferior direction with the thumbs, so as to depress the transverse processes (TP) of T1 and the adjoining first ribs (Fig. 9). In CCP, the left TP is more superior than the right and resists the operator's downward forces, suggesting a right sidebending of T1.
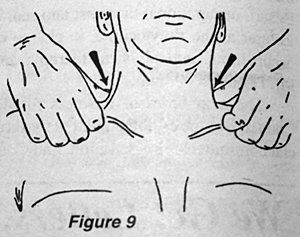
If treatment were undertaken at this point with the aforementioned data, two separate maneuvers would be required. T1 would have to be rotated left with one procedure and also sidebent back to neutral with a compensatory left lateral flexion secondary procedure.
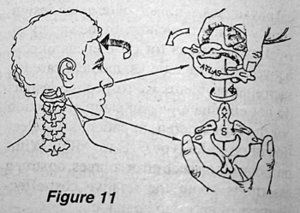
In CCP, the neck is sidebent left, creating a mild left-sided concavity or dextroscoliotic curve. The examiner should rotate the neck to the right and left (Fig. 10).
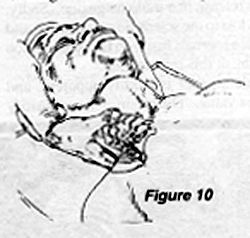
In CCP, the upper cervical complex should rotate more easily to the left, suggesting that the upper cervical segments are malpositioned in left rotation (Fig. 11). The upper cervicals should also sidebend easier to the right, suggestive of a right lateral flexion malposition.
Next, the examining physician should extend the arms upward over the head of the patient. In CCP, the right arm will appear longer, reflecting the torsional stresses of the thoracic cage and inequality of eccentric shoulder girdle muscular contraction.
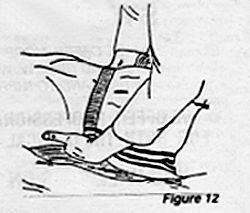
A general idea of the lumbar lordotic curve can be obtained by sliding the flat of the hand under the back of the supine patient. It will not appear as prominent as it would if the patient were standing upright, back to the wall. But with practice, the physician will get a "feel" for the normal lordotic supine presentation (Fig. 12).
This paper has conveyed information, developed within the osteopathic profession, regarding the recumbent postural exam. The common compensatory pattern was described and it was used as a working model to enhance the description of the supine postural exam. Therefore, utilization of a recumbent postural exam as part of the total structural exam gives the examiner a rapid diagnosis leading to appropriate utilization of osteopathic manipulative therapy. One would bear in mind that while we most often find the CCP during the supine postural examination, other configurations may also be observed and as always the total clinical presentation should be evaluated. Alternate configurations have been referred to by Zink as disparent patterns.
Bibliography
Christensen K: Clinical Chiropractic Biomechanics. Educational Division of Foot Levelers, Inc., Roanoke, VA, 1st Ed., 1984.
Christensen K: Clinical Chiropractic Orthopedics. Educational Division of Foot Levelers, Inc., Roanoke, VA, 1st Ed., 1984.
Cross N, Johnson K: Lumbar facet angle asymmetries in racially distinct populations. JAOA, 1990, 90:929.
Cyriax J: Orthopaedic Medicine, Vol. II. Baillier Tindall 1 St. Anne's Rd. Eastbourne, East Sussex, BN21 3UN 11th Ed., 1984.
Fryette H: Principles of Osteopathic Technique. AAO, 1954.
Johnson K, Cross N: Common compensatory pattern and its relation too lumbar facet angles. JAOA, 1990, 90:942.
OP&P Depart., University of New England College of Osteopathic Medicine, OMT Course Notes, 1991-2.
Kapandji IA: The Physiology of Joints. Vol. 3. Churchill and Livingston, 1974.
Schafer RC, et al.: Basic Chiropractic Procedures Manual, 4th Ed. Associated Chiropractic Academic Press. ACA, Arlington, VA, 1984.
Schneider W, et al.: Manual Medicine Therapy. Thieme Medical Publishers, New York, 1983.
Stodard A: Manual of Osteopathic Practice. 2nd Ed. Hutchinson and Co., 17-21 Conway St., London W1P 6JD, 1983.
Stodard A: Manual of Osteopathic Technique. 3rd. Ed. Hutchinson and Co., 17-21 Conway St., London W1P 6JD, 1980.
Zink JG, Lawson W: An osteopathic structural examination and function interpretation of the soma. Osteopathic Annals, 7:12 Dec. 1979.
Guy Defeo, DO
Laurence Hicks, DC
N. Berwick, Maine



